Peripheral artery disease and intermittent claudication
Highlights
Peripheral Artery Disease
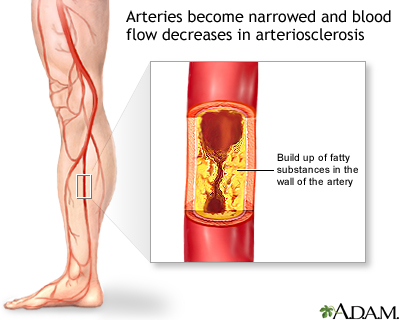
Peripheral artery disease (PAD) is a type of atherosclerosis. It occurs when arteries in the limbs (most often the legs) become narrowed by cholesterol-rich material called plaque. Because PAD interferes with circulation, advanced cases increase the risk for gangrene and amputation. Patients with PAD are also at increased risk for other types of atherosclerosis, including heart attacks and strokes.
Risk Factors of PAD
The main risk factors of PAD include:
- Smoking
- Diabetes
- Unhealthy cholesterol and lipid levels
- High blood pressure
- Advancing age
Symptoms
Many people with PAD do not have symptoms. When symptoms do occur, crampy leg pain (intermittent claudication) is the main symptom. This symptom occurs off and on, usually with exercise, and disappears when at rest. When PAD becomes more severe, symptoms can include:
- Pain or tingling in the feet or toes, even at rest
- Weakened calf muscles
- Painful non-bleeding ulcers on the feet or toes that do not heal
Treatment
Treatment for PAD includes both lifestyle measures and medications that help reduce symptoms and prevent disease progression. These include:
- Smoking cessation
- Regular exercise, which is essential for patients with mild-to-moderate PAD
- Heart-healthy diet, low in saturated fat, to reduce unhealthy cholesterol levels
- Medications to help control high blood pressure and cholesterol. Other drugs that may help include antiplatelet medications to prevent blood clots.
- In severe cases, procedures may be needed to open blocked blood vessels.
Introduction
Peripheral artery disease (PAD) occurs when the arteries in the extremities (usually legs and feet, sometimes arms and hands) become clogged with a fatty substance called plaque. It most often occurs in the legs. The build-up of plaque causes the arteries to become narrow and hard, obstructing blood flow. This hardening of the arteries is called atherosclerosis. (Atherosclerosis that affects arteries to the heart and brain is the major process leading to heart disease and stroke.)
PAD is a type of peripheral vascular disease, which also includes carotid artery disease, renal artery disease, aortic disease, venous problems, and some other conditions, such as vasculitis.
Symptoms
People with peripheral artery disease (PAD) may or may not have symptoms. Because of symptoms may be mild or even absent, many cases of PAD go undiagnosed.
Intermittent Claudication
Claudication comes from the Latin word "to limp." Claudication is crampy leg pain that occurs during exercise, especially walking. The pain is due to insufficient blood flow in the legs (caused by blocked arteries). Intermittent means the pain comes and goes. Intermittent claudication is the most prominent symptom of PAD. About a third to a half of patients with PAD have this symptom.
Symptoms may be felt as pain, achiness, cramping, a sense of fatigue, or nonspecific discomfort that occurs with exercise. There is no discomfort while standing. Symptoms go away rapidly with rest, usually within a few minutes. At first, symptoms may only initially develop when walking uphill, walking faster, or walking longer distances.
Because the most frequently affected artery in intermittent claudication is the popliteal artery, symptoms are most common in the calf muscles. This artery leads off from the femoral artery (the major artery in the thigh). It continues below the knee where it branches off and carries blood to the muscles in the calf and foot. Talk to your doctor about any leg or thigh pain you have.
Leg pain occurs in one leg in 40% of patients and in both legs in 60% of patients. Patients may also have fatigue or pain in the thighs and buttocks.
Advanced Peripheral Artery Disease (Ischemic Rest Pain)
In advanced cases, the arteries are so blocked that even rest does not help. Leg pain that continues when lying down is called ischemic rest pain. Ischemia is the medical term for insufficient blood flow to tissues.
Typical symptoms may include:
- Pain or tingling in the foot or toes, which may be so severe that even the weight of clothes or bed sheets cause or worsen the discomfort
- Pain worsens when leg is elevated and improves by dangling legs over the side of the bed
People with ischemic rest pain are at risk for ulcers and gangrene. In severe cases, amputation may be required.
Other signs of advanced PAD can include:
- Calf muscles that shrink (wither)
- Hair loss over the toes and feet
- Thick toenails
- Shiny, tight skin
- Painful non-bleeding ulcers on the feet or toes (usually black) that are slow to heal
Sometimes, blood clots form in the arteries in the legs, producing abrupt symptoms.
Risk Factors
About 8 million American adults have peripheral artery disease (PAD). Men and women are equally susceptible although women face a greater risk for limb loss. African-Americans have twice the risk for PAD as Caucasians. Between 12 - 20% of people over age 65 suffer from the condition.
PAD Risk Factors
The most important risk factors for PAD are the same as those for heart disease and stroke. Smoking and high cholesterol levels increase the risk for PAD progression in large blood vessels (such as the legs), while diabetes increases the risk for PAD in small blood vessels (such as the feet). Quitting smoking and controlling cholesterol are the two best ways to slow PAD progression.
The most important risk factors for PAD include:
- Smoking. Smoking is the number one risk factor for PAD, and smoking even a few cigarettes a day can interfere with PAD treatment. Smoking increases the risk for PAD by 2 - 25 times, with the danger being higher when other risk factors are present. Between 80 - 90% of patients with PAD are current or former smokers. Progression to a more critical state of illness is likely for patients who continue to smoke. [For more information, see In-Depth Report #41: Smoking.]
- Diabetes. People with type 2 diabetes have 3 - 4 times the normal risk for PAD and intermittent claudication. In fact, their risk for PAD is higher than their risk for heart disease. People with type 2 diabetes also tend to develop PAD at an earlier age and have more severe cases. Patients with both diabetes and PAD are at high risk for complications in the feet and ankles. Poor blood sugar (glucose) control increases the risk of developing PAD. [For more information, see In-Depth Report #60: Diabetes - type 2.]
- Unhealthy cholesterol and lipid levels. The risk for PAD increases by 5 - 10% with every 10 mg/dL increase in total cholesterol levels. Levels of HDL ("good cholesterol") below 40 mg/dL and high triglyceride levels also increase the risk for PAD. LDL ("bad cholesterol") levels should be kept below 100 mg/dL in all patients with PAD, and probably as low as 70 mg/dL when other risk factors are present (such as diabetes, coronary artery disease, smoking, and HDL below 40 mg/dL). [For more information, see In-Depth Report #23: Cholesterol.]
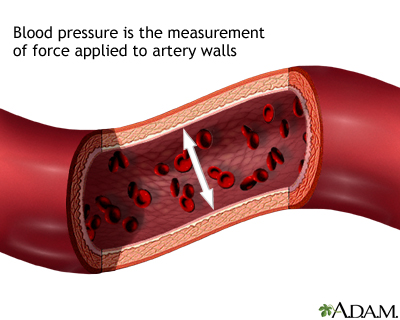
- Hypertension. High blood pressure, especially when combined with other cardiovascular risk factors, increases the chances for PAD. [For more information, see In-Depth Report #14: High blood pressure.]
- Family history of heart and artery disease. Genetic factors that cause specific lipid and cholesterol abnormalities may increase the risk for PAD.
- Artery inflammation and damage. High levels of C-reactive protein can indicate persistent inflammation in the arteries. Such inflammation can cause significant damage in blood vessels, and is highly associated with PAD.
- Age. PAD occurs more frequently in people over age 50 and affects 12 - 20% of Americans age 65 years and older.
- Ethnicity. African-Americans are at highest risk for PAD. They are twice as likely to develop PAD as Caucasians.
Diagnosis
PAD is greatly underdiagnosed. Many patients do not report symptoms, or may not even have symptoms. People should be checked for peripheral artery disease if they have leg pain during walking, or ulcers on their legs.
Physical Examination
The doctor should check for high blood pressure, heart abnormalities, blockage(s) in the artery in the neck, and abdominal aneurysms. The doctor should also examine the skin of the legs and feet for color changes, ulcers, infection, or injuries, and check the pulse of the arteries in the leg.
Ankle-Brachial Index
Intermittent claudication caused by peripheral artery disease is typically diagnosed using a calculation called the ankle-brachial index. This method also helps to diagnose PAD in patients without symptoms of intermittent claudication.
The procedure is done as follows:
- The doctor or technician measures the systolic blood pressure of both arms while the patient is lying down. (The systolic pressure is the "top" number in a blood pressure measurement. It is the force that blood exerts on the artery walls as the heart contracts to pump out the blood. For example, in a blood pressure reading of 120/80, 120 is the systolic number.)
- The doctor or technician then puts blood pressure cuffs on four different locations on each leg and passes a Doppler probe over arteries in the foot. The signal emitted from the strongest artery is recorded as the cuffs are inflated and deflated. This is the ankle's systolic pressure.
The doctor divides the systolic pressure in the ankle by the systolic pressure in the arm. The result is called the ankle-brachial index (ABI), also called ankle-arm pressure index (API).
What the results mean:
- ABI over 0.90. A normal ABI can range from 0.90 to 1.30. In general, an ABI result over 1.0 is considered normal and results from 0.91 to 0.99 are considered borderline. If results fall in the borderline range, and the patient has specific risk factors for artery disease, the patient takes a treadmill test and another ABI measurement. If the API index drops, the doctor makes a diagnosis of peripheral artery disease.
- ABI 0.40 – 0.80. These measurements indicate moderate impairment and symptoms such as leg pain.
- ABI less than 0.40. These measurements indicate very severe blockage in the leg arteries and a risk for gangrene. Patients should take precautions to avoid foot injuries, which can increase the risk for non-healing wounds and gangrene.
Doppler Ultrasound Imaging
Doppler ultrasound imaging is commonly the first imaging test of the arteries performed and also may be used in follow-up of patients. It is able to provide an anatomic view of the arteries and report on velocity and flow characteristics. It is non-invasive and is usually performed in an outpatient setting.
Invasive Angiography, Magnetic Resonance Angiography (MRA), and Computed Tomography Angiography (CTA)
Before considering invasive procedures to treat peripheral artery disease, the surgeon needs a better understanding of which arteries are involved, how severe the blockage is, and the state of the blood vessels surrounding the blockage. In the past, invasive or conventional angiography was typically performed. This type of angiogram uses dye, which is injected through a catheter that is inserted in the groin.
Magnetic resonance angiography (MRA) is a type of magnetic resonance imaging (MRI). It provides a non-invasive alternative to a traditional angiogram. The MRA uses a magnetic field and radiofrequency waves instead of radiation to provide pictures of arteries and blood vessels. Patients are given gadolinium (a contrast material) through an IV to improve the image quality. In many medical centers, MRA is considered almost or as accurate as invasive angiography and will frequently be the only test required.
A newer technology called computed tomography angiography (CTA) uses x-rays to visualize blood flow in arteries throughout the body. This technique is also highly effective in diagnosing PAD. While it involves radiation exposure, it can be used in patients who have contraindications to magnetic resonance imaging.
Treadmill Test
A patient is often given a treadmill test if the ankle-brachial index is questionable. Patients with claudication have a 50 - 60% reduction in peak performance, which is comparable to that in patients with heart failure. The treadmill test is also useful for determining the severity of the pain while walking and assessing the effectiveness of treatments.
Waveform Analysis
A test called a wave form analysis may be used to confirm an abnormal API or pressure reading. The patient lies on their back for at least 10 minutes in a warm room (so that the blood vessels will not narrow). The leg is turned outward, and the knee is slightly bent. The doctor passes a handheld scanner over the leg, which picks up sound waves coming from the arteries. These signals are recorded, and the wave forms are traced to detect abnormal blood flow.
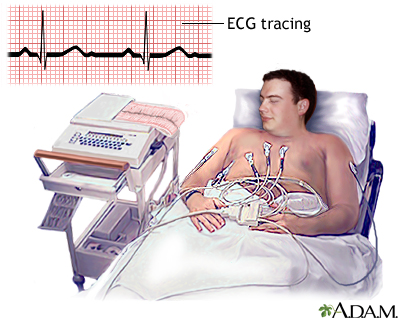
Tests for Detecting Heart Disease
Patients with suspected PAD should have an electrocardiogram (ECG, EKG) and other tests that can detect heart problems.
Ruling out Other Disorders with Similar Symptoms
A number of other tests may be ordered to rule out disorders with similar symptoms. Such disorders include:
- Arthritis
- Anemia
- Spinal stenosis -- narrowing of the spinal canal causing leg or lower back pain
- Thrombophlebitis -- blood clots in the deep veins of the legs
- Peripheral neuropathy -- nerve damage in the legs and feet, usually in people with diabetes
- Night cramps in older people that are not due to problems in blood vessels
- Muscle entrapment of the arteries or kinks in the arteries in the leg -- typically occurs in young athletes
Complications
Coronary Artery Disease and Stroke
Patients with peripheral artery disease (PAD) have the same risk of death from heart events or stroke as people already diagnosed with heart disease. The risk increases as PAD gets worse. The worse the leg condition, the poorer the overall health of the patient.
If patients have blood clots and blockages in other arteries (brain, heart) as well as the legs, the risk for any vascular complication involving the heart, the brain, or the leg arteries increases much more.
Acute Occlusion
In rare cases, blood clots can develop suddenly in a major artery in the leg -- a condition called acute occlusion. Symptoms include numbness, pain, coolness, pale color, lack of pulse in the artery, and weakness. This is a very serious event, which can lead to amputation or even loss of life. Treatment options include clot-busting drugs delivered to the blockage or procedures to remove the clot.
Poor Physical and Mental Functioning
Peripheral artery disease can significantly impair daily physical functioning. Claudication pain severely limits physical activity. Even worse, intermittent claudication increases the risk for falling, usually because of unsteadiness, regardless of the severity of PAD. Intermittent claudication and PAD are also associated with mental decline.
Treatment
There are two treatment goals for PAD and claudication:
- Manage the pain of intermittent claudication, improve functioning, and prevent PAD from getting worse, so that gangrene does not occur.
- Reduce the risk for cardiovascular disease (heart attack and stroke).
Lifestyle changes, especially smoking cessation and exercise, are critical for every patient with PAD. Medication is often required to improve function and protect the heart. In very severe cases, surgery may be needed to improve blood flow.
Treatment for PAD also involves managing the medical conditions (diabetes, high cholesterol, and high blood pressure) that often accompany it.
Managing Diabetes
Patients with diabetes need to strictly control their blood sugar (glucose) levels. Poor glycemic control is associated with vascular and circulation complications such as PAD. Patients should aim for an A1C level around 7%. The AIC test measures a patient’s average blood sugar over the past 2 - 3 months. Patients with diabetes need to follow certain dietary restrictions. Many different types of medications are used to control blood sugar levels. [For more information, see In-Depth Reports #60: Diabetes type 2, #09: Diabetes type 1, and #42: Diabetes diet.]
Managing Unhealthy Cholesterol and Lipid Levels
It is very important for people with PAD to keep their LDL ("bad" cholesterol) levels to below 100 mg/dL. If patients have serious heart disease risk factors (high blood pressure, diabetes, other unhealthy lipids) in addition to PAD, they may need to aim for LDL levels below 70 mg/dL. Unhealthy cholesterol levels are major contributors to atherosclerosis, the common factor in PAD and heart disease. Patients should avoid saturated fats and foods that are high in cholesterol. A statin drug may is the most common type of medication used to help lower LDL cholesterol and improve lipid profiles.
Statins include:
- Lovastatin (Mevacor, generic)
- Pravastatin (Pravachol, generic)
- Simvastatin (Zocor, generic)
- Fluvastatin (Lescol)
- Atorvastatin (Lipitor, generic)
- Rosuvastatin (Crestor)
- Pitavastatin (Livalo)
[For more information, see In-Depth Report #23: Cholesterol.]
Managing High Blood Pressure
In addition to dietary measures to reduce sodium (salt) and increase potassium intake, various medications are used to control high blood pressure (hypertension). Patients with PAD should aim for blood pressure less than 130/80 mm Hg.
Evidence suggests that the best drugs for patients with high blood pressure and PAD are angiotensin-converting-enzyme (ACE) inhibitors. These drugs block the effects of the angiotensin-renin-aldosterone system, which is associated with many harmful effects on the heart and blood vessels. They are important drugs for patients with PAD and diabetes who also have high blood pressure. In addition to heart protection, ACE inhibitors may help reduce pain that patients experience when walking.
ACE inhibitors include:
- Captopril (Capoten, generic)
- Enalapril (Vasotec, generic)
- Quinapril (Accupril, generic)
- Benazepril (Lotensin, generic)
- Ramipril (Altace, generic)
- Perindopril (Aceon, generic)
- Lisinopril (Prinivil, Zestril, generic)
[For more information, see In-Depth Report #14: High blood pressure.]
Lifestyle Changes
Quit Smoking
Patients who smoke should quit, and everyone should avoid second-hand smoke. Smoking is one of the primary risk factors for PAD and a major cause of complications. Quitting smoking may not make leg pain go away, at least not in the short term, but it certainly may keep blockages from getting worse. Continued smoking is associated with the majority of patients who progress from milder forms of PAD to critical limb ischemia involving severe pain, skin ulcers, and possible amputation. Smoking cessation also reduces the risk to the heart.
Exercise
Exercise is second only to avoiding tobacco as the most important lifestyle measure for treating, and preventing, PAD.
Exercise to Help the Heart. The benefits of regular moderate exercise for the heart are undisputed. People who maintain an active lifestyle have a much lower risk of developing heart disease than do sedentary people. And, according to the American Heart Association, patients with PAD who are physically active have death rates that are a third of those who are less physically active.
Exercise Training to Improve Blood Flow in the Legs. Exercise training improves blood flow in the legs and, in some cases, can work as well as medications and surgical procedures in increasing pain-free walking distance. To maintain benefits, exercise must be regular and consistent. A regular walking program, either outside or on a treadmill, is the best type of exercise for patients with PAD and can significantly slow the rate of functional decline.
For patients with intermittent claudication who find that their leg cramps make it difficult to walk or participate in lower-extremity exercise, upper-body aerobic exercise can still provide benefits.
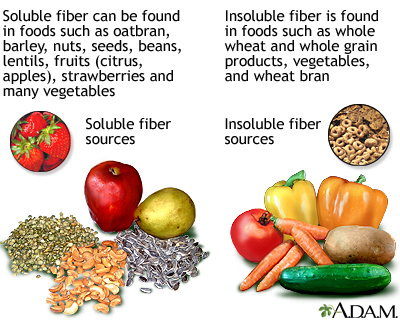
Eat Healthy
The goals of a heart-healthy diet are to:
- Reduce overall cholesterol levels and low-density lipoproteins (LDL), which are harmful to the heart
- Increase high-density lipoproteins (HDL), which are beneficial for the heart
- Reduce other harmful lipids (fatty molecules) such as triglycerides and lipoprotein(a)
Any diet should also help keep blood pressure and weight under control. General guidelines for a heart-healthy diet include:
- Choose fiber-rich food (such as whole grains, legumes, and nuts) as the main source of carbohydrates, along with a high intake of fresh fruits and vegetables.
- Avoid saturated fats (found mostly in animal products) and trans fatty acids (found in hydrogenated fats and many commercial baked products and fast-foods). Choose unsaturated fats (particularly omega-3 fatty acids found in vegetable and fish oils).
- When selecting proteins, choose soy protein, poultry, and fish over meat.
- Weight control, quitting smoking, and exercise are essential companions of any diet program.
[For more information, see In-Depth Report #43: Heart-healthy diet.]
Vitamins
Vitamins have not been proven to reduce the risk for PAD or heart disease. Low levels of vitamin D have been linked to an increased risk of PAD and many older Americans are deficient in this vitamin. More research is needed to determine if vitamin D supplements protect against PAD. Deficiencies in the B vitamins folate and B12 have been linked with elevated levels of homocysteine, an amino acid that has been associated with a higher risk for heart disease and PAD. However, while vitamin supplementation lowers homocysteine levels, it has no effect on heart disease outcomes. Vitamin E has also not been shown to help with symptoms.
Herbs and Supplements
Generally, manufacturers of herbal remedies and dietary supplements do not need FDA approval to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been a number of reported cases of serious and even lethal side effects from herbal products. Always check with your health care provider before using any herbal remedies or dietary supplements.
Gingko biloba is an herbal remedy reported to have blood-thinning properties. However, studies have shown it does not provide any benefit for patients with PAD or intermittent claudication. Although the risks for gingko appear to be low, there is an increased risk for bleeding at high doses and harmful interaction with high doses of anti-clotting medications. This is particularly important because patients with PAD often use these types of medications. Commercial gingko preparations have also been reported to contain colchicine, a chemical that can be harmful in pregnant women and people with kidney or liver problems.
Medications
Treatments for PAD help manage leg pain and improve function, as well as reduce the risk for heart attack and stroke. Drugs used for improving leg pain and function are generally those that either prevent blood clots (typically antiplatelet drugs) or improve blood flow.
Aspirin and Other Antiplatelet Drugs
Antiplatelet drugs such as aspirin reduce the risk for blood clots. Most patients with peripheral artery disease receive antiplatelet medication. For the most part, this recommendation is made to prevent future death from heart attack or stroke. (However, recent studies have indicated that aspirin may not have much benefit in preventing heart attack or stroke in patients who have PAD without also having heart disease.) Antiplatelet drugs may or may not provide benefit for PAD symptoms and progression.
Aspirin is usually the recommended first-line choice. Clopidogrel (Plavix, generic) is recommended as an alternative.
Dipyridamole (Persantine, generic) may help prevent complications of PAD when taken along with aspirin. Studies are mixed on the benefits of the combination. Without aspirin, the drug does not appear to have any advantages for patients with PAD.
Research indicates that adding an anticoagulant drug, such as warfarin (Coumadin, generic), to antiplatelet therapy does not help prevent heart complications of PAD, and can increase the risks for life-threatening bleeding.
[For more information on these drugs, see In-Depth Report #03: Coronary artery disease.]
Phosphodiesterase Inhibitors
Phosphodiesterase inhibitors are drugs that help improve blood flow.
Cilostazol. Cilostazol (Pletal, generic) is used to treat disabling intermittent claudication. A number of studies have reported that the drug helps improve walking distance and quality of life. It also helps improve HDL and triglyceride levels. Cilostazol works better than pentoxifylline, the first drug approved for claudication. It is expensive, however, and currently recommended only for patients with moderate-to-severe intermittent claudication who do not respond to aspirin or less costly treatments. Common side effects include headache, swelling in the limbs, and stomach problems such as diarrhea and flatulence (gas). It does not appear to have bad effects on the liver or kidney. Similar drugs have had serious side effects in patients with heart failure, so these patients should avoid cilostazol.
Pentoxifylline. Pentoxifylline (Trental, generic) reduces the sticky properties of blood, improving its flow. It is approved in the U.S. for managing claudication, although doctors do not recommend its routine use. Studies regarding the drug's effectiveness have been mixed. Some studies have reported a small effect on walking ability; another found the drug significantly improved walking distance. Other research has found that the drug does not work any better than a dummy pill (placebo). The most common side effects include headache, nausea, heartburn, flatulence (gas), dizziness, blurred vision, and flushing.
Thrombolytics (Clot-Busters)
Alteplase (Activase), also called t-PA, and reteplase (Retavase) are thrombolytic drugs. Such drugs are commonly called "clot-busters." They break up existing clots, and may be used in cases of acute vascular occlusion (the sudden development of a blood clot). They may also be used if a clot is present. Researchers are investigating whether thrombolytics are an effective alternative to surgery in severe cases of PAD. In severe cases, the drugs can be delivered directly into the artery.
Other Drugs Used to Treat Intermittent Claudication
ACE Inhibitors. ACE inhibitors are a type of drug used to treat high blood pressure. The ACE inhibitor ramipril (Altace, generic) is often recommended for patients with symptomatic peripheral artery disease, primarily to reduce the risk of cardiovascular events.
Surgery
In severe cases, surgery may be needed to open blocked blood vessels. Many surgical procedures can be performed. These include open bypass procedures, which connect an artery before the location of the obstruction to an artery below the obstruction, or minimally invasive endovascular techniques such as angioplasty and stenting. The location of the lesions and how many other risk factors and illnesses patients have often determine which procedure is chosen.
Surgery is generally performed for claudication that has become disabling despite full medical and exercise therapy. Surgery may also be necessary for patients with rest pain, and to save a limb when a patient develops critical limb ischemia and is in danger of amputation.
Leg Bypass Surgery
For many years, leg bypass surgery was the main type of surgery used for extensive PAD. This procedure involves the creation of a tube (graft) that acts as a new blood vessel. Grafts can be made from synthetic material (artificial vein) or from a vein taken from a different location in the patient's leg (natural vein). The graft reroutes blood flow in the leg, around the blocked artery. Possible bypass connections between arteries include aorta to iliac arteries, aorta to femoral arteries, and bypass between the femoral artery and popliteal, tibial, and peroneal arteries.
Artificial veins tend to pose a much higher risk for blood clots, and the consequences of re-blockage are must more severe than when the natural vein recloses. To keep the artificial vein open, oral anti-clotting drugs such as aspirin or warfarin may be used. (Such drugs do not work with natural vein bypass.)
In general, less invasive procedures, such as balloon angioplasty and stenting, are now more frequently performed.
Percutaneous Transluminal Angioplasty
Percutaneous transluminal angioplasty (PTA) is an approach that has several variations. The object of the procedure is to open the blocked blood vessels that are causing intermittent claudication. Angioplasty is being increasingly used in place of leg bypass surgery, especially in patients who have other medical conditions.
The PTA procedure requires only a local anesthetic. Patients can return to normal activity in 24 - 48 hours. Complication rates are low. The effects are not permanent, but the procedure can be repeated without any greater risk than with the original one.
Anticoagulants (such as warfarin or heparin) and antiplatelets (such as aspirin) may be used to prevent blood clots occurring during surgery. All of these drugs increase the risk for bleeding. Thrombolytic drugs may be used before, during, or after angioplasty if a blood clot is present.
Balloon Angioplasty. The standard procedure is balloon angioplasty. A thin tube is inserted through an artery in the groin and passed through the blocked artery. A wire is threaded through the tube. A deflated balloon is passed over the wire to the blockage. When inflated, it opens the artery.
Because of the risk for reclosure from blood clots after balloon angioplasty, various other procedures are used or are being investigated.
Stenting. Reblockage of the blood vessels from blood clotting, even long after surgery, is an important complication. To help prevent this complication, and repeat surgery, a tiny expandable metal mesh tube (stent) is often used along with angioplasty. However, even with stents, some patients experience new blockages within a year of surgery. Some angioplasties are performed with a drug-eluting stent, which is coated with the drug paclitaxel to help prevent artery blockages.
Drug-eluting stents may not be recommended for patients who had recent heart surgery, or women who are nursing or pregnant. Patients who receive a drug-eluting stent may need blood thinning drugs for at least several months.
Resources
- www.padcoalition.org -- Peripheral Arterial Disease Coalition
- www.nhlbi.nih.gov -- National Heart, Lung, and Blood Institute
- www.heart.org-- American Heart Association
- www.acc.org -- American College of Cardiology
- www.diabetes.org -- American Diabetes Association
- www.vdf.org -- Vascular Disease Foundation
- www.sirweb.org -- Society of Interventional Radiology
References
Aboyans V, Criqui MH, Denenberg JO, Knoke JD, Ridker PM, Fronek A. Risk factors for progression of peripheral arterial disease in large and small vessels. Circulation. 2006 Jun 6;113(22):2623-9.
Alonso-Coello P, Bellmunt S, McGorrian C, Anand SS, Guzman R, Criqui MH, et al. Antithrombotic therapy in peripheral artery disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e669S-90S.
Arain FA, Cooper LT Jr. Peripheral arterial disease: diagnosis and management. Mayo Clin Proc. 2008 Aug;83(8):944-49; quiz 949-50.
Aung PP, Maxwell HG, Jepson RG, Price JF, Leng GC. Lipid-lowering for peripheral arterial disease of the lower limb. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD000123.
Berger JS, Krantz MJ, Kittelson JM, Hiatt WR. Aspirin for the prevention of cardiovascular events in patients with peripheral artery disease: a meta-analysis of randomized trials. JAMA. 2009 May 13;301(18):1909-19.
Collins R, Burch J, Cranny G, Aguiar-Ibáñez R, Craig D, Wright K, et al. Duplex ultrasonography, magnetic resonance angiography, and computed tomography angiography for diagnosis and assessment of symptomatic, lower limb peripheral arterial disease: systematic review. BMJ. 2007 Jun 16;334(7606):1257. Epub 2007 Jun 4
Creager MA and Libby P. Peripheral arterial disease. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; 2012:chap 61..
Fowkes FG, Price JF, Stewart MC, Butcher I, Leng GC, Pell AC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010 Mar 3;303(9):841-8.
Garg PK, Tian L, Criqui MH, Liu K, Ferrucci L, Guralnik JM, et al. Physical activity during daily life and mortality in patients with peripheral arterial disease. Circulation. 2006 Jul 18;114(3):242-8.
Hamburg NM, Balady GJ. Exercise rehabilitation in peripheral artery disease: functional impact and mechanisms of benefits. Circulation. 2011 Jan 4;123(1):87-97.
Hirsch AT, Allison MA, Gomes AS, Corriere MA, Duval S, Ershow AG, et al. A Call to Action: Women and Peripheral Artery Disease: A Scientific Statement From the American Heart Association. Circulation. 2012 Mar 20;125(11):1449-1472. Epub 2012 Feb 15..
McDermott MM, Ades P, Guralnik JM, Dyer A, Ferrucci L, Liu K, et al. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA. 2009 Jan 14;301(2):165-74.
Met R, Bipat S, Legemate DA, Reekers JA, Koelemay MJ. Diagnostic performance of computed tomography angiography in peripheral arterial disease: a systematic review and meta-analysis. JAMA. 2009 Jan 28;301(4):415-24.
Olin JW, Allie DE, Belkin M, Bonow RO, Casey DE Jr, Creager MA, et al. ACCF/AHA/ACR/SCAI/SIR/SVM/SVN/SVS 2010 performance measures for adults with peripheral artery disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures, the American College of Radiology, the Society for Cardiac Angiography and Interventions, the Society for Interventional Radiology, the Society for Vascular Medicine, the Society for Vascular Nursing, and the Society for Vascular Surgery (Writing Committee to Develop Clinical Performance Measures for Peripheral Artery Disease). J Am Coll Cardiol. 2010 Dec 14;56(25):2147-81.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012 Jan 3;125(1):e2-e220. Epub 2011 Dec 15.
Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, et al. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease (updating the 2005 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011 Nov 1;58(19):2020-45. Epub 2011 Oct 6.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT,Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011 Nov 29;58(23):2432-46.Epub 2011 Nov 3.
Warfarin Antiplatelet Vascular Evaluation Trial Investigators, Anand S, Yusuf S, Xie C, Pogue J, Eikelboom J, et al. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007 Jul 19;357(3):217-27.
|
Review Date:
5/24/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |





